|
|
|
|
Chapter
9
Health And Health Services

A Concert Party at Ludham Manor
in the 1940s. On the left chair is
Mary Leadsom, Ludham District Nurse in the 30s
and 40s
|
The
health and medical services of the parish should be
viewed in the context of the radical social and
political changes of the 20th Century in Britain as a
whole. The first half of the century saw the passing
of Acts of Parliament paving the way to the
establishment of the Welfare State which, after the
wartime Beveridge report of 1941/2, culminated in the
final repeal of most of the remnants of the Poor Laws
in 1948. (vide appended chronology table).
Medical and surgical progress was being made as the
century advanced. Infectious diseases were the
dominant cause of death in the first half of the
century, but, even prior to the advent of antibiotics
just before the second world war, progress was being
made in the control of tuberculosis by means of public
health measures such as Xray screening, better housing
and diet, combined with isolation and treatment of
sufferers in sanitaria.

|
On 5th July 1948 The NHS was born.
When health secretary Aneurin Bevan launched
the NHS at Park Hospital in Manchester (now
known as Trafford General Hospital), it was
the climax of a hugely ambitious plan to bring
good healthcare to all. For the first time,
hospitals, doctors, nurses, pharmacists,
opticians and dentists were brought together
under one umbrella organisation to provide
services that were free for all at the point
of delivery. The central principles were
clear: the health service would be available
to all and financed entirely from taxation,
which meant that people would pay into it
according to their means. |
|
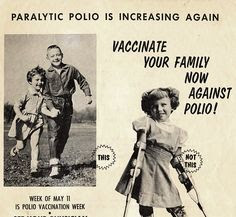
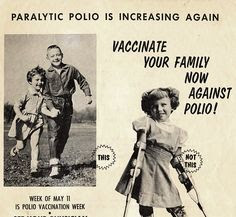
Antibiotics played a dramatic role in
the improvement of prospects in acute
bacterial infections such as pneumonia,
scarlet fever and rheumatic fever, and
immunisation programmes springing from the
public health machinery established under the
Welfare State progressively reduced the
incidence of tetanus, poliomyelitis,
diphtheria in the 1950’s and whooping cough
and measles later on in the 60’s. All these
programmes were largely implemented by local
medical practitioners, as had smallpox
vaccination been in the previous century.
National screening programmes were set up for
cervical cancer in the early1970’s which was
also largely GP based, and later on for breast
cancer (hospital based). Cancer treatments
also became much more effective in the closing
decades of the century. Hospital surgical
techniques improved commencing with successful
operations for acute abdominal emergencies
such as appendicitis and perforated peptic
ulcers in the early years of the century,
progressing to open cardiac surgery and
transplant surgery in the 60’s, and
culminating in extraordinary ‘key-hole ‘
procedures more recently. |
The century saw the arrival of electricity in the
village from Norwich (1926-8), piped water from the
wartime system of RAF Ludham (1955) and mains drainage
and sewage treatment. The latter was installed during
the war for RAF Ludham and the military camp in School
Lane had its own separate system on land which is now
part of Willow Way. The new council houses in School
Lane were connected to the RAF treatment plant at
‘Pooh Corner’ in 1952, and finally the service was
extended to the rest of the village in 1972 by
Smallburgh Rural District Council. All of these
services were of obvious benefit to the health and
wellbeing of the Parish.
Before sewage treatment was made available to the bulk
of the village, households relied on septic tanks, or
the weekly night time visit by the ‘honey-cart’ (the
latter district council service continued well into
the 80’s for some outlying properties!). Water had
been mainly drawn from wells, but there was also a
protected spring near Manship Cottages which served
adjacent properties; the Manor and Manor Bungalow
continued to use a well until it was sucked dry by the
water extraction plant used to lower the water table
for deep sewer mains installation in 1972, and an
emergency water supply had to be laid on! Some
outlying cottages were not connected to electricity
for up to quarter of a century after its first arrival
in the area, and Nurse Pettitt sometimes had to
deliver babies by oil light and without the benefit of
running water in the early fifties!

Staithe House
Dr. Gordon, a prosperous Irish practitioner, started
our century for the medical profession, having
purchased the Ludham practice from Dr Samuel Taylor
Huke, MRCS LSA in 1879, together with the Manor
House from which he practiced, where there was a small
surgery at the back of the house. He appears to have
been a wealthy man and is said to have owned a herring
drifter at Yarmouth, as well as being a local
magistrate. He also owned the old staithe which
enabled boats to load and unload alongside Staithe
road. There was a bitter dispute around 1904
-1906 between him and the parishioners over access to
the staithe, which he eventually successfully
enclosed, having taken the case to law, allegedly
using perjured witnesses!

Lime Kilns at the old staithe
The only reminder of the past economic importance of
the staithe is the remains of an old lime kiln
standing in the riverside garden of Barn Owl Cottage
(formerly in the garden of Staithe House).
His paying patients were the better off members of the
community such as tradesmen farmers and professional
people; many working families belonged to contributory
medical clubs and friendly societies, such as The
Ancient Order of Foresters and Oddfellows, whilst the
poor were entitled to treatment under the Poor Law
provisions.
In the first decade of the 20th century about 20% of
the population belonged to medical clubs and up to 10%
were paupers. GP’s served the Poor Law boards as
medical officers and Dr Gordon was officially a
‘district surgeon’ to the Smallburgh Union. The 1911
Lloyd George National Insurance Act extended sickness
insurance to all employees, but still under the
independent sector. ‘Approved Societies’, which
were often friendly societies or trade unions,
administered the system when it came into effect in
1913, but by 1930 things had become much more
commercialised.
The societies created the GP ‘panels’ of insured
patients which in due course would form the nucleus of
the National Health practices of 1948. However,
dependents were not covered, and hospital treatment
was not routinely included. Some of the societies
offered hospital care as an optional extra, but as
late as 1939 less than 10% of the 18.6 million insured
nationally were so covered. In Norfolk 30% of the
population were entitled to free GP access just after
the Insurance Act, rising to 40% by 1939. One local
resident recalls the exact contribution his mother
made to their health insurance society agent when he
called, which was sixpence a week (2.5 new pence) – “a
penny each and tuppence for the family”!
A major part of Dr Gordon’s work would probably have
been domestic, and of course included obstetric
emergencies when summoned by local midwives. Rural
doctors income varied considerably, and no record of
Dr Gordon’s medical income has come to light, but
published research indicates that at the turn of the
century an annual average for GPs in Norfolk was in
the order of £1000 gross, with about a quarter coming
from medical clubs and poor law contracts.
<PICTURE> 05 catfield rectory.jpg

Catfield
Rectory
|
Dr Evelyn Kempson Brown took over in
1918, when Dr Gordon retired to Gorleston, and
practised from his home at Staithe House. He
had previously been in practice in Dorset for
16 years, and was invited by Dr Gordon to take
over the practice. They knew each other well
as Dr Brown had been brought up in Catfield
where his father was Rector for many years.
The Rector himself educated all of his twelve
children at home, and Evelyn was the youngest:
from an early age he was determined to be a
doctor, and his father finally agreed and sent
him to train at the London Hospital, where he
lived in digs costing 12/6 (62.5 new pence) a
week! |
The Rector’s living, a good one for Norfolk, was about
£600 per annum. Once qualified, Dr Brown married at
quite a young age for the time, as it was thought that
married doctors were more trustworthy and hence would
be more likely to be financially successful! He
borrowed £200 from his father in law which was
sufficient to establish himself in practice in
Cranbourne in Dorset at the turn of the century.
When he returned to his native county,
he moved up with his family in their two
cylinder Swift motor car which his daughters
remember well, and was one of the first in
Ludham! His wife had planned to train as a
nurse, and helped him out in the surgery when
assistance was needed, although by and large
doctors managed on their own in those days.
The patients attending surgeries had to wait
outside on the river side of Staithe House,
but apparently could observe progress through
a small window in the Surgery door! Memories
also remain of his skills at dental extraction
– without anaesthesia - a recognised part of a
GPs work in those days before there were many
dental surgeons. The practice still has a full
set of traditional dental forceps handed down
by an earlier doctor.
|

|
Recollections of the 1918/9 influenza pandemic
(‘Spanish Flu’) were that, although Dr Brown was busy,
he was not overwhelmed. Doctors were of course on-call
24 hours a day and holidays were infrequent – about
every four years in Dr Brown’s case, as locums had to
be paid, housed, and fed! Mrs Brown on one occasion
won £600 in a lottery, and this paid for a holiday in
Germany for Dr Brown who spoke fluent German, and
later another in Scotland with all the family. It was
during this holiday that they met a Swiss family who
were to remain life long friends, and the encounter
explains the unusual inscription on his grave in the
church yard close to the National School Room –‘uf
wiederluge’ (German Swiss dialect for ‘auf
wiedersehen’) Apparently he also held the post of
Registrar locally, not an unusual arrangement at that
time. During his three decades working in Ludham, his
best ever gross annual income was £1300.

Red Roof Farm
|
Dr Brown retired rather reluctantly in
his mid seventies, moving with his wife to a
bungalow on his son-in law’s Red Roof farm at
Potter Heigham, and two of his daughters still
live in the village at the time of writing.
Peter Wilson took over at Staithe House,
enlarging Dr Brown’s small surgery on the
river side of the house, by adding a waiting
room! He saw the introduction of the NHS in
1948; GPs remained self-employed but reached
agreement on complicated contracts for
reimbursement with the Ministry of Health,
which guaranteed treatment free at the point
of delivery to all patients. Sale of the
goodwill of medical practices ceased, but GPs
were allowed to join the NHS pension scheme as
a quid pro quo, which enabled subsequent
generations to retire at a more reasonable age
if they so wished! Dr Wilson was respected by
his patients, who often recalled his edicts
many years later. He was actively involved in
local and national political activity with the
British Medical Association and took on Dr
Bolt as an assistant, and later partner, in
order to give him time for this activity and
the growing practice; finally he departed to
BMA HQ in London, handing on the practice to
Dr Gabriel, who had become his partner when Dr
Bolt returned to hospital practice. Whilst
working at the BMA, Dr Wilson helped to
negotiate the 1965 Family Doctor Charter with
the government, which offered financial
incentives to GPs to improve their surgery
facilities and employ ancillary staff and for
which we have cause to be very grateful to
him, as the Ludham practice was able to
benefit from the opportunities offered. Before
he left the practice there had been another
influenza pandemic (‘Asian Flu’) in 1957/8. |
| Dr Gabriel lived at Stalham Green as
junior partner, and started a small surgery
attached to his house there, which Dr Edmonds
took over and expanded in 1972 when appointed
following Dr Wilson’s departure, Dr Gabriel
moving to Staithe House (Dr Jeremy Meanley had
come before Dr Edmonds for a few months as
assistant-with-a-view, but decided not to
stay). In 1965/6 Dr Gabriel added a timber
extension to the Staithe House surgery, which
included a new consulting room facing Womack,
and conversion of the old consulting room to a
dispensary, so that he had space for a
receptionist/dispenser to work. (the Wilson
& Gabriel extensions were demolished after
Dr Gabriel’s retirement and move to the Manor
in 1984, but the concrete base can still be
seen). Following the 1965 Family Doctor
Charter, Dr Gabriel employed the first
ancillary medical staff in the person of Mrs
Edna Grapes as secretary; later staff were
recruited for reception and dispensing duties.
Another major influenza pandemic (‘Hong Kong
Flu’) struck in 1968/70, and Dr Gabriel
remembers the first call coming as he was
about to carve the Christmas turkey – he
finally got back to eat late that evening, and
the epidemic took several weeks to pass. |

Dr Gabriel
|
In 1973/4 Ludham nearly lost its NHS medical practice
when the County Council, who at that time played a
major role in local health-care provision, started
negotiations with all the local GPs with a view to
building a health centre in Stalham, which would have
resulted in the closure of all outlying surgeries,
including Ludham. However, the agreement of all of the
local GPs was not forthcoming and events were
overtaken by government reforms which removed much
health care provision from local government control in
1974. As an alternative to the need for better medical
facilities, and lacking the availability of a suitable
central site in Stalham, the Department of Health
‘Cost-Rent’ scheme of the 1965 Charter was exploited
in 1976/7 to build a new purpose-designed surgery in
Ludham on a piece of land belonging to the Manor just
up the road from the old surgery, with Michael Innes,
of Castle Mall fame, as architect.

Ludham Surgery
|
By this time there were four
ancillary staff, Iris Gibbs, Margaret
Bullock, Shirley Meek, and Jenny Tann, and
Dr Jarvis had joined the practice as a third
partner in 1971, having previously come as a
trainee-assistant for a year. The expansion
in ancillary staff was exponential over the
ensuing years, and a list is appended – the
practice had 11.67 full time equivalents by
the time it appointed a new practice manager
in the vanguard of yet another New Contract
with the Department of Health in 2004.
|

Dr Jarvis
|
Unusually, it did not employ nurses directly as the
district nurses (employed by the local health
authority after 1974) worked very closely with the
practice, including work in the surgery which, after
the 1990 New Contract, included nurse practitioner
contract work related to chronic disease management.
Dr Savage replaced Dr Gabriel on the latter’s
retirement in 1982, and later Dr Sudlow joined as a
part time fourth partner, having worked as an
assistant under the government Retainer Scheme (a full
list of partners is appended as part of the
Chronology).
Dispensing was always an important duty of general
medical practitioners in rural Norfolk, and in
previous centuries their usual title had been that of
surgeon/apothecary: physicians (with ‘Oxbridge’
degrees) were confined largely to wealthy urban areas.
The adoption of the title of general practitioner only
gradually became the norm following the Medical
Registration Acts of the 19th century
This dispensing role was recognised in the 1948
National Health Service Act and GP dispensing
continued under contracts with the new local health
authorities (‘Executive Councils’) established by the
Act. Up until the move to the new surgery in 1977,
when the surgery was closed, prescriptions were left
out on a shelf in the entrance lobby of the surgery
for patients to collect at their convenience: the door
was never locked, and the service was never abused!
After the start of the NHS, licensed pharmacists
(established by the 1852 & 1863 Pharmacy Acts)
were seen by GPs as a threat to their lucrative
dispensing practice, as pharmacists were entitled
under the new arrangements to take NHS dispensing
rights from GPs for those patients living within a
mile of their pharmacy. Ludham did not have a
pharmacy, and the only threat to the doctors came from
a pharmacy in Stalham which, although it had been
established in 1836 (largely for vetinary work), only
started NHS dispensing when taken over by David
Coleman FPS in 1962, much to the chagrin of the
Stalham GP Dr Jimmy Walsh and his local colleagues
including Dr Gabriel at Stalham Green!

Norfolk &
Norwich Hospital
|
Supplies of drugs, dressings and
appliances were delivered to the practice by
various Norwich wholesalers. In the first part
of the century a lot of medicines were
compounded by the doctors from stocks of
ingredients and before the 1970’s, deliveries
were usually weekly, but with the explosion of
new effective, but expensive, drugs in the
latter quarter of the century, more frequent
replenishment of stock became imperative, and
by the end of the century twice daily
deliveries had been established. Similarly,
pathological samples, which had been delivered
in person to the hospital laboratories in
Norwich, or put on the bus at Thrower’s for
collection by the hospital from the St
Stephen’s bus depot, were in the latter two
decades of the century collected from the
surgery by a daily hospital collection
service. In fact, during the first 60 years of
the century no pathological specimen service
existed, and patients had to be referred to
the Norfolk & Norwich Hospital consultant
pathologist in person, in the event of tests
being required which were beyond the scope of
the GP. |
Doctors before Dr Gabriel had entered general practice
without specific specialist training, usually straight
after qualifying from medical school – after 1948 a
compulsory pre-registration year in hospital was added
after qualification, and in the 1950’s a voluntary
year’s Trainee Assistant Scheme was initiated -
doctors serving as resident assistants to an
established practitioners rather like an
apprenticeship, and Drs Gabriel, Edmonds and Jarvis
all held such training positions – in the case of Dr
Jarvis this was at Ludham under Dr Gabriel’s tutelage,
and accommodation for him and his family was provided
in the Manor Bungalow.
| A national three year training
programme in general practice was developed in
the 1970’s – two years in hospital and one in
practice with day release teaching at the
local post graduate medical teaching centre
(Norfolk & Norwich Institute of Medical
Education–NANIME-established by the Ministry
of Health paper HM(64)69 and located in the
teaching centre in the 1771/2 building of the
Norfolk & Norwich Hospital from 1973 until
the hospital moved to Colney in 2001). This
training became compulsory in 1982, by which
time the Trainees had been renamed Registrars
in line with hospital specialty trainee
colleagues. Dr Savage was the first doctor at
Ludham to have been previous trained under
this scheme and five years after his arrival
took on the role of Trainer when the Practice
was approved to become a teaching practice
once more (a list of trainees & registrars
is appended). |

Norfolk and
Norwich Hospital
|
Other admissions to hospital prior to 1980 were mainly
surgical (acute and planned surgery) and medical beds
were scarce; most medical emergencies such as heart
attacks and strokes as well as the terminally sick
were cared for at home, with the aid of the resident
district nurse and her neighbouring colleague in
Hickling (see case study on the nursing role of Miss
Betty Pettitt). In those days the nurses were dual
trained as midwives and general nurses, and in the
case of Sister Pettitt, the long time Ludham resident
nurse, as Health Visitor as well. Home visits were
much more frequent, and surgery attendance lighter –
until the move to the new surgery there was no
appointment system, and a full waiting room had a
deterrent effect on the faint hearted! With the 1990
New Contract, much more emphasis was put on GP Chronic
Disease Management. asthma & diabetes clinics were
established followed by screening for, and closer
structured supervision of, these and other chronic
medical problems. Meanwhile the hospitals had been
steadily expanding their service to acute medical
cases, easing the domiciliary care load of GPs,
although to some extent this has been offset by the
rapid expansion of private Nursing and Residential
Care Homes in the last two decades of the century
which occurred as direct result of the government
initiating reimbursement of the private sector for
residential care. Previously this had been provided by
county council social services departments through
‘Part 3’ homes, such as Sydney House in Stalham (built
c1960 to replace and modernise the old poor law
provision of residential accommodation such as the
Lingwood workhouse, which has been taken over by
Norfolk County Council as the poor laws were
dismantled).

The Old
Vicarage Nursing Home
|
In Ludham, the Old Vicarage became a
nursing home in about 1980, and other new care
establishments in Sutton, Hickling, Catfield
and Potter Heigham came under the medical care
of the Ludham Practice.
|
Improved communications systems and
computerisation have played a dramatic role in
the extended provision of health care: public
telephones appeared in the first quarter of
the century, and were initially resented by
practitioners, who felt that they made it too
easy for the doctor to be summoned at night!
Previously a runner had to be sent to the
doctor’s house, and Staithe House still has a
‘Night Bell’ push below the normal house bell.
Pressing this used to ring a bell in the
doctors bedroom – apparently he would usually
then stick his head out of the window above
and question the runner as to the urgency of
the call! A minority of homes had telephones
before 1970, and surgeries were blissfully
uninterrupted by the telephone ringing – any
requests for house calls had to be brought or
telephoned to the doctors housekeeper before
morning surgery! Now the doctors have an army
of staff to handle the ever increasing
telephone call load.
When out on visits, doctors were
difficult to contact before many homes had
telephones, and several attempts were made in
the 70’s to use early paging services, but
these proved to have many shortfalls. In 1988
NARS, through the good offices of the Eastern
Daily Press, and an overwhelming response from
the public to their ‘Rescue Radios’ appeal,
established its own two-way radio system,
which served both for practice and ambulance
calls, and proved to be of immense value over
the next 15 years.
|

|
The future of the provision of health care at parish
level is difficult to foresee; many will regret the
passing of the personal 24 hour service which the
Ludham doctors had provided throughout the 20th
century. However advances in delivery of emergency
care by the local ambulance trust has provided a
consistent and suitable alternative closely linked to
local hospital emergency units. Despite being less
personal, this offers definite advantages in terms of
resuscitation and certain emergency treatments such as
‘clot- busters’ for heart attacks. Advances have been
dramatic in preventive medicine at a local level as
well as in diagnostic technology and therapeutic
improvements in our local hospitals. Continuation of a
surgery in the village looks secure, but as in 1973/4,
local health decisions might move towards
centralisation of primary health care facilities,
nothing is guaranteed.
The District Nurse - Betty Pettitt
(1928 - 2017)

Betty Pettitt
|
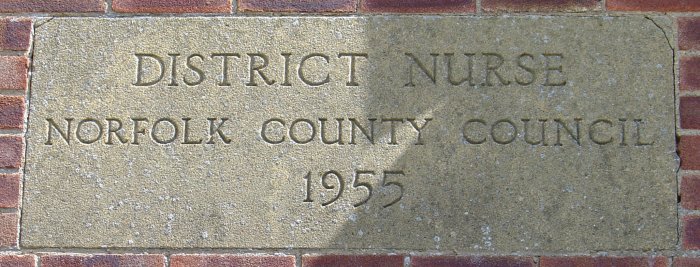
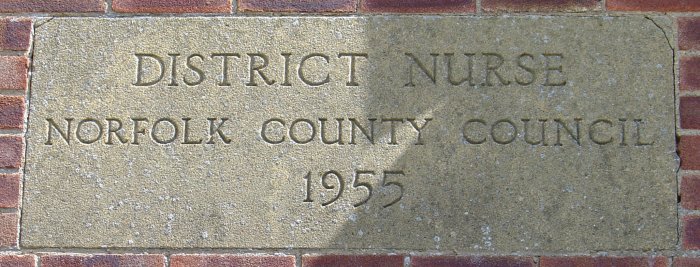
Betty Pettitt came to Ludham in
1955. She was qualified as a State
Registered Nurse and a State Certified
Midwife. In the same year she took her
Queen’s Institute of District Nursing
Certificate, and in 1958 – 59 she completed
her Health Visitor training. Prior to her
arrival, her predecessors were trained only
in midwifery.
She was
appointed by the Norfolk County Council
District Nursing Service and her salary
followed national rates, an annual amount
divided into twelve equal parts. Housing had
to be provided, as it was a requirement of
the job that the nurse lived in the area
where she worked. A house was built on
School Road, but until it was completed, the
nurse lived in the council bungalow next
door. She moved into the Nurses House in
1956, and paid rent starting at £1 a week.
This increased year by year and was deducted
directly from her salary.
|
Her appointment was to the post of District Nurse,
Midwife and Health Visitor to Ludham, Catfield and
Potter Heigham. All her equipment was provided, but
she had to buy drugs that were needed in her midwifery
work, from the chemist, and apply for reimbursement
afterwards.
Prior to the founding of the National Health Service,
many villages had their own District Nursing
Association, which was controlled by a committee of
local ladies. Villagers paid a small amount of money
each week to enable them to have the District Nurse or
Midwife visit them when necessary. The Treasurer
for many years was Mrs. Boardman from How Hill, and
because of her long standing connection with the
Association, she had been allowed to administer the
petty cash, which she did until she died. The nurse
had to visit her every two to three months in order to
claim the money she had spent on items such as drugs.

District Nurse House. School Road
The area in which the nurse worked was enlarged soon
after her appointment, to include Horning, Neatishead,
Barton Turf, Smallburgh and Dilham. At first, off-duty
time was half a day per week, beginning at 2,00 p.m.
and finishing at 10.00 p.m. This was increased over
the years. Local nurses worked in groups of three or
four to cover each other’s time off. In this respect,
the nurse at Ludham worked with nurses covering Repps,
Martham, Winterton, Somerton, Thurne, Oby and
Clippesby.
To enable satisfactory coverage of these quite
considerable distances, cars could be provided, but
the nurse in Ludham had her own and claimed a mileage
allowance. Nurse Pettitt worked with and for General
Practitioners. In the 1950’s there were two doctors
working at Ludham, but others from Wroxham, Stalham,
Smallburgh and Martham also had patients in the
village, because areas overlapped. This caused
confusion at times, as nurses were not allowed to
cross their area boundaries.
As a trained midwife, the Ludham nurse was a
practitioner in her own right, and could administer
drugs such as Entonox and Oxygen for the baby.
Until this time, these had not been available to
mothers in labour.
(Entonox, or sometimes referred to as ‘laughing gas’,
has been used in the NHS since 1965 for relieving pain
and anxiety. It is a mixture in equal parts of nitrous
oxide and oxygen, and is commonly used in childbirth
and by the ambulance service for the relief of pain.
Entonox works very quickly and its effects are felt
almost immediately after inhalation, making it a very
good pain relief with a relaxing effect without losing
consciousness or control. It is self-administered via
a patient controlled on-demand facemask and
mouthpiece, leaving the patient in full control of
their own pain relief requirements. The effects of the
Entonox gas will be felt after approximately 6-8
inhalations. After stopping inhalation, the gas and
its effects wears off quickly, and within eight
minutes it will have disappeared completely from the
body.)
The main part of the nurse’s work concerned midwifery.
The majority of mothers had their babies delivered at
home. Both midwife and doctor would be present if
possible, in case things went wrong, but this was not
always possible. The G.P. and nurse provided antenatal
care, and together they established the first
antenatal clinic.

|

|
At the time when a telephone in the home was a rarity
it was mainly public call boxes that were used, but
the police often had to be used to get urgent messages
delivered when the nurse was away from home. Betty
Pettitt had her father living with her and he often
took messages, but otherwise she wrote on a small
blackboard the places where she expected to be, with
estimated times, and this was placed in a window in
her house.
Nursing Officers in Norwich had control over local
nurses. One such officer would visit every three to
four months to examine the books; the Drugs and
Nursing Registers. Once a year an officer accompanied
the nurse on her morning rounds to check that her work
was up to scratch.
From 1955 to 1974 Nurse Pettitt combined the three
parts of her work, General Nursing, Midwifery, and
Health Visitor, which also included the job of School
Nurse. Off duty time also increased year by year. In
1974 Local Health Authorities came into existence and
the service was reorganised. It was taken away from
the County Council, and the practical result was that
all three services were divided into separate units,
which made it much more difficult for the nurse to
keep three registers. As a result, Nurse Pettitt
became a full time Health Visitor, in her own area.
Her other duties were carried out by a new District
Nurse and a new District Midwife. By this time, G.P.s
were putting boundaries on their practice areas, so
the nursing and midwifery staff could work from a
surgery and mainly with one practice. This was a big
change for someone who had previously worked from
home.
SOURCES
Bruce, Maurice, The Coming of the Welfare State,
Bruce, Batsford Ltd 1961
Muncaster, M J., Medical Services and the
Medical Profession in Norfolk 1815-1911. PhD thesis
for University of East Anglia 1976
Gabriel, Dr DW., Edmonds, Dr DA., Townsend, Mrs
N., Brown, Miss R., Fuller, Mr M., Gowing,
Mrs B., Kittle, Mr C., Osbourne, Mr R.,
Boldy, Mrs Y., Thrower, Mr T., and many other Ludham
residents, past and present, personal communications
1970-2006
Cherry, Steven, Pennies for the Healthcare, printed by
UEA, 1993
Maynard, Tracey (former Practice Manager, currently
Quality Control Manager) preparation of practice staff
lists and illustration of Staithe House Surgery site
Battyshaw, Dr Anthony, Norfolk and Norwich
Medicine, 1992, Norwich Medico-Chirurgical Society
(ISBN 0 9518866 0 6 hardback)
Snelling, Joan, Ludham: A Norfolk Village
1800-1900, E. Mumby, 1999
GLOSSARY OF MEDICAL QUALIFICATIONS
LSA
Licentiate of the Worshipful Society of Apothecaries
LM
Licentiate in Medicine
LRCP
Licentiate
of the Royal College of Physicians (London or
Edinburgh)
LRCS
Licentiate of the Royal College of Surgeons
(Edinburgh)
MRCP
Member of the Royal College of Physicians (London)
MRCS
Member of the Royal College of Surgeons (London)
MB BS(or Ch
B)
Bachelor of medicine and surgery
MRCGP
Member of the Royal College of General Practitioners
FRCP
Fellow of
the Royal College of Physicians
FIMC RCS
Ed
Fellow of the Royal College of Surgeons Edinburgh
(immediate care)
D(Obst)RCOG/DRCOG
Diploma (Obstetrics) of the Royal College of
Obstetricians and Gynaecologists
DFFP/MFFP
Diplomate/Member of the Faculty of Family Planning and
Reproductive Health RCOG
MRCS LRCP was known as the ‘conjoint’ qualification,
necessary for registration after the 1886 Medical Act,
and later superseded by the Universities’ conjoined
degrees in medicine and surgery: however, it remained
a valid qualification - as did LSA (which until 1869
had been the only diploma examining in midwifery – the
RCS then began to include it in their examination for
membership). Conjoint and LSA were amalgamated into
the United Examinations Board diploma (UEB) towards
the end of the century and finally abolished in 2000.
CHRONOLOGY OF PRINCIPAL DOCTORS IN THE LUDHAM
PRACTICE
AND IMPORTANT MEDICAL DATES OF RELEVANCE
1900-2000
1879-1918 James
Alexander Gordon JP LRCP LRCS
(Edin) LM
1903
Kelling
Sanitarium built (Public TB Hospital)
1911
The National
Insurance Act (created insurance panels of patients
which would in 1948 become the core of GPs’ NHS lists)
1918-1947 Evelyn
Kempson Brown MRCS LRCP
1923
North Walsham
War Memorial Cottage Hospital built: GP hospital.
Separate maternity unit added later but converted in
mid 1990’s to
Primary Care
Centre for out of hours work.
1926-8
Electricity arrives in the
village.
1929
The Local
Government Act (local authorities assumed the role of
Poor Law Boards)
1947-1964 Peter
Remington Wilson MA MRCGP MRCS
LRCP
1941/2
The Beveridge Report;
blueprint for the Welfare State which the post-war
socialist government implemented, leading to:-
1948
The Start of the
National Health Service
1952
Foundation of
the College of General Practitioners in London
Council houses in
school lane linked to military base/RAF sewage system
1955-1959
Geoffrey Leon Bolt VRD MB BS FRCP
(Assistant 1953-54) appointed as second partner
1955
Piped water
provided for most of the parish from the RAF system
adjacent to their sewage treatment plant on the
Catfield road
1959-1982 David
Wilson Gabriel MB BS MRCGP
1962
Leo House
Surgery built, Stalham Green
1965-1997 Duncan
Alexander Edmonds MB BS D(Obst)RCOG
1965
The Family
Doctor Charter. Negotiated between BMA &
Government: provided financial support for the
development of purpose-built surgeries,
and partial reimbursement of ancillary staff funding
1971-2002 Robert
James Terry Jarvis MB ChB FIMC
RCSEd MFFP&D(Obst) RCOG (Trainee Assistant
1970-1971) appointed as third partner
1972
Mains Drainage
installed in the parish by Smallburgh RDC
1977
Silver Jubilee
Queen Elizabeth II. Building of the new surgery
in the Manor grounds, Staithe Road, Ludham.
Closure of Hickling Branch
surgery a year later
1982
James Smallwood
Savage MB BS MRCGP DRCOG
1987
Two storey
extension of Ludham Surgery
1989
Sheila Sudlow
BSc MB ChB MRCGP DRCOG (Assistant
1987-1988) Appointed as fourth partner
1990
The New GP
Contract. Radical reform of Health Department’s
requirements of general practice, followed by
computerisation of the practice to
facilitate
compliance with new government audit requirements etc.
1993
Building of the
new surgery on the site of Pond House, Yarmouth Road,
Stalham Green
1997
Andrew Colin
Buchanan Sale MA MB BS MRCGP
DFFP & DRCOG (Trainee 1995-1996)
2000
End of UNITED
EXAMINATION BOARD (Conjoint & LSA)
LUDHAM MEDICAL PRACTICE ANCILIARY STAFF IN 20th
Century
Grapes Edna 1966-70
Boyce Eileen 1969-70
Priest Rita 1970-1975
Butcher (Rushmer) Judith 1971-1972
Attmere (Smith) Lynn 1972-2000
Roberson Freda 1974-6
Hanbury Betty 1978-1982
Gibbs Iris 1975-1990
Meek (Ellis) Shirley 1975-1977 & relief to 78
Bullock Margaret 1977-2000
Tann (Steggles) Jenny 1976-1977
Thomas Brenda 1977-2000
Phillips Marjorie 1977-1989
Clarke (Wolstenholme) Rosemary (Practice Manager)
1977-1993
Cuddington Joy 1982-1992
Richardson Diane 1986-July 1989
Jones Sally 1989-1997
Kay Grace (relief) 1987-2000
Blogg Jenny 1990-2000
Maynard (Edwards) Tracey (Practice Manager from
1993)1991-2000
Monsey (Dalton) Julie 1993-2000
Ward Julie 1998 -2000
Mills Sandra 1999-2000
Morris Margaret 1997 -2000
COMMUNITY STAFF ATTACHED TO LUDHAM SURGERY
Betty Pettitt District Nursing Sister/Midwife/Health
Visitor 1955 - 1985
Joan Gettings District Midwife 1985-2000
Rosemary Wilson HV 1985-1990
Ruth Warner HV 1990-2000
Teresa Hales District Nursing Sister 1975 -2000
Annie Palmer District Staff-Nurse 1989-2000
Annette Dore Community Physiotherapist 1989-2000
|
|
|